Degenerative-dystrophic diseases of the spine, or more simply, osteochondrosis, not only affects a growing number of the adult population on our planet, but also makes them much younger. Today, more than 80% of the working-age population on our planet is periodically disturbed by spinal pain.
Osteochondrosis- a disease of the spine that results in degenerative-dystrophic damage to the intervertebral discs and the underlying bone tissue, with thickening of the vertebral processes and loss of elasticity of the ligaments along the spine. This leads to aging, dehydration and loss of cartilage tissue stability.
Osteochondrosis is not only a deterioration in spinal pain or limb tenderness, but a disease of the whole body. And as many studies show, osteochondrosis has a direct effect on virtually all internal organs. For example, cervical spine disorders affect the functioning of the organs of vision, hearing, mental, and mental activity. In the chest region, the work of the cardiovascular system, the gastrointestinal tract is disrupted. Degenerative-dystrophic changes in the lumbar spine lead to organ problems in the pelvis, includingthe urogenital area and lower extremities. For example, in the same lower limb are accompanied by various pains, muscle cramps, "creeping creeps", numbness of the limbs and subsequent atrophy. Therefore, early detection and qualified treatment of this pathology is very important. Many people who are first diagnosed with intervertebral hernia are confronted with the choice of methods for their treatment. The proposal for surgical treatment leaves many in a state of shock, forcing them to seek alternative therapies. Some immediately turn to traditional healers, bone builders, others take various medications, others do nothing at all, insisting on the view that the disease should be treated when it is very worrying. In this regard, neurosurgeons have a winged expression: "walking with a hernia is like walking with a grenade, no one knows when it will explode! " But unfortunately, surgical treatment, be it neurosurgery or orthopedics, is not a panacea. In many patients, spinal pain persists after surgery, which is associated with the development of cicatricial adhesions, and relapses (recurrence of the disease after apparent recovery of the disease ("recurrence")) - recurrent hernias - often occur.
In osteochondrosis, the intervertebral discs are most commonly affected. These unique cartilage washes not only connect our 33 vertebrae to the spine. Its good working conditions, mobility, flexibility, flexibility, load resistance depend directly on the condition of the intervertebral discs. They serve as spring dampers to dampen the load.
Osteochondrosis occurs as early as the first decades of life and has been observed to be more common in boys than in girls.
If left untreated to prevent and treat osteochondrosis, the disease progresses, gradually affecting the entire spine, which can ultimately lead to disc herniation, nerve endings, and stinging of parts of the spinal cord. In severe cases, the consequences of osteochondrosis can only be eliminated by surgery with a long recovery and rehabilitation period.
Types of osteochondrosis
Depending on the part of the spine affected by the disease, the following types of osteochondrosis are distinguished:
- Cervical osteochondrosisor osteochondrosis of the cervical spine.
- Chest osteochondrosisor osteochondrosis of the thoracic spine.
- Lumbar osteochondrosisor osteochondrosis of the lumbosacral spine.
- Common osteochondrosis,in which case the disease spreads to two or three parts of the spine at once.
- First:the main symptom of osteochondrosis at this stage is instability, manifested in the initial abnormalities of the vertebral discs. You feel bad and uncomfortable.
- Second:the main symptom of the second stage of osteochondrosis is protrusion of the disc. Destruction of the annulus fibrosus begins, the gaps between the vertebrae are reduced, and it is possible to tighten the nerve endings with pain syndromes.
- Third:at this stage of osteochondrosis, ring destruction occurs with the appearance of intervertebral hernias. The third stage is characterized by significant deformity of the spine.
- Fourth:the last and most severe stage of osteochondrosis. It will be hard to move. Any movement leads to acute pain. From time to time, the condition improves and the pain subsides, but this is a clear indication of the development of bone growth. They connect the vertebrae, restrict the ability to move, and lead to disability.
There are four stages of development of osteochondrosis
Symptoms of osteochondrosis
Patients with osteochondrosis complain of persistent painful back pain, often accompanied by numbness and pain in the limbs. In the absence of proper treatment, weight loss and limb atrophy occur. The main symptoms are:
- persistent painful back pain, numbness, and limb pain;
- increased pain with sudden movements, physical exertion, weight lifting, coughing and sneezing;
- decreased range of motion, muscle cramps;
- with osteochondrosis of the cervical spine: pain in the arms, shoulders, headache; the possible development of the so-called vertebral artery syndrome, which consists of the following complaints: noise in the head, dizziness, flashing "flies", colored spots combined with throbbing headaches burning in the eyes. Vertebral artery syndrome can be caused by spasms, which can be traced back to direct irritation of the sympathetic plexus due to bone growth, disc herniation, arthrosis of the intervertebral joint, and irritation of any receptor in the spine. The presence of vertebral artery syndrome may exacerbate the course of coronary or cardiovascular pathology, if any;
- with osteochondrosis of the thoracic spine: pain in the chest (as a "stake" in the chest), in the region of the heart and other internal organs;
- with osteochondrosis of the lumbosacral spine: back pain, radiating to the sacrum, lower extremities, sometimes to the pelvic organs;
- damage to nerve roots (with herniated intervertebral discs, bone growths, spondylolisthesis, spondyloarthrosis): shooting pain and impaired sensitivity, hypotrophy, hypotension, weakness of innervated muscles, decreased reflexes.
Diagnosis of osteochondrosis
The preliminary diagnosis is made during the initial examination of the patient. The examination is usually performed by a neurologist in connection with the patient's complaints about local complaints, which may present as pain, deformity, or restriction of movement. The spine is examined with the patient standing, sitting, and lying down, both at rest and in motion. The level of spinal lesion is determined by the number of vertebrae from certain anatomical features or according to a special scheme.
When examining the back, pay attention to the posture, structural features of the trunk, mark the line of vertebral processes (middle groove of the back), lower angles of the shoulder blades, the spine of the hip bones, the lateral side of the waist and neck, the deviation of the groove from the vertical shows a revelation, the protrusion of the vertebral processes pays attention to the relief of the muscles located next to the spine.
Spinal sensation allows the examination data to be supplemented (presence or absence of deformity) to determine the localization, extent, and nature of the pain. When palpated, the tension of the muscles adjacent to the spine should also be noted. most spinal injuries and diseases are accompanied by increased muscle tone.
Spine flexion is used to determine the range of motion in different parts of the spine.
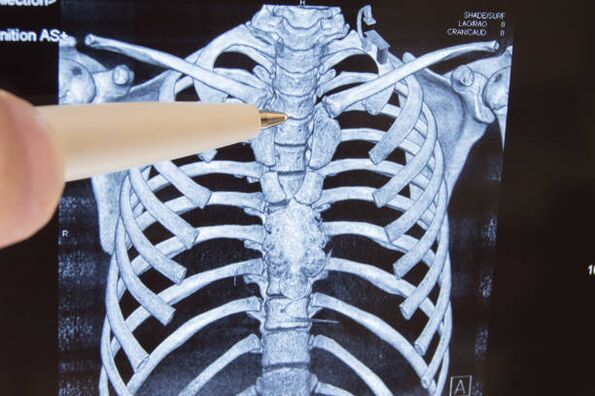
The main role of spinal examination is radiography, computed tomography, and magnetic resonance imaging, which help determine the level of the lesion, clarify and concretize the diagnosis, and uncover hidden pathologies. Diagnostic data allow the treating physician to determine treatment tactics and select the most effective treatment methods.
Osteochondrosis of the spine, treatment with movement
Complex conservative treatment includes physiotherapy practices, physiotherapy, massage, manual therapy, spinal traction (reflexology), reflexology, drug therapy.
Physiotherapy exercises (exercise) - the main method of conservative treatment of musculoskeletal disorders, the creation of dosed loads aimed at decompression of nerve roots, correction and strengthening of the muscle ligament, increasing the volume and development of a certain stereotype. movements and correct posture, giving the ligament-muscular devices the flexibility they need and preventing complications. This is accomplished through regular exercises with rehabilitation equipment and joint gymnastics. As a result of the exercise, blood circulation is improved, the metabolism and nutrition of the intervertebral discs are normalized, the intervertebral space is increased, the muscle ligament is formed and the load on the spine is reduced.
Physiotherapy is a method of treatment that uses physical factors: low frequency currents, magnetic fields, ultrasound, laser, and so on. It is used to relieve rehabilitation after pain, inflammation, injuries and surgeries. With the use of physiotherapy methods, the treatment time of many diseases is shortened, the efficiency of the use of drugs and the reduction of their dosage is increased, and drug treatment has no side effects.
Massage is a set of mechanical dosing methods in the form of friction, pressure, vibration, performed directly on the surface of the human body by hand. Effectively relieves muscle tension, muscle pain, improves blood circulation, has a tonic effect.
Manual therapy is an individually tailored manual effect on the musculoskeletal system to relieve acute and chronic pain in the spine and joints, as well as increase range of motion and correct posture. One direction of manual therapy is visceral manual therapy, which helps to restore normal mobility of organs, improves blood supply, lymphatic circulation, normalizes metabolism, restores immunity and prevents the exacerbation of chronic diseases.
Spinal traction (traction) is an effective method of treating spinal and joint pain syndromes using an individually selected load using special equipment. The procedure aims to increase the intervertebral space, relieve pain and restore the anatomically correct shape of the spine.
Reflexotherapy - various therapeutic techniques and methods to affect the reflexogenic zones of the human body and acupuncture points. The use of reflexology in combination with other therapeutic methods significantly increases their effectiveness. Reflexology is most commonly used for osteochondrosis, accompanied by pain, nervous system diseases, sleep disturbances, mental imbalances, and overweight and smoking. By acting on certain points, you can harmonize your body and treat many diseases.
Drug therapy is indicated during exacerbation of the disease, with the aim of relieving pain, relieving the inflammatory process, and enhancing metabolic processes by taking drugs by intramuscular or intravenous injection.
Although all of the above methods are extremely effective, a lasting therapeutic effect can only be achieved when combined with the practices of rehabilitation devices to create a full-fledged muscle bandage.
Recommendations for the prevention and prevention of osteochondrosis
To prevent osteochondrosis or reduce pain, people with the disease are advised to have a situation for as long as possible in which the load on the intervertebral discs is minimal, while the back muscles need to be stretched. to support metabolic processes around the spine. The general recommendations range from following the rules of a healthy lifestyle, and in each case the doctor will determine the private recommendations.
To prevent this, the following rules must be observed:
- Do not overload the spine, do not create conditions that promote increased pressure on the intervertebral discs:
- limits vertical loads;
- do not perform sudden movements, especially body turns;
- avoid falls and jumps from a height, injuries and bruises on the spine;
- change your body position more often;
- keep your back straight;
- try to maintain the natural physiological curves of the spine: in a supine position, the load on the spine is minimal, but the bed should be semi-rigid (preferably sleeping on a solid orthopedic mattress and orthopedic pillow); in a sitting position, keep your back straight because of the muscles, or push to the back of a chair or chair (the seat should be hard enough and your back should bend in the lumbar region), keep your head straight; when standing still, change the leg you are leaning on more often; getting up from a bed or a chair and lying down and sitting down must be done by hand without straining or bending your back;
- drink water and massage your back before physical activity, this will scatter blood, speed up metabolic processes, and allow intervertebral discs to absorb enough moisture;
- do not lift or hold heavy objects on outstretched arms, lift an object, squat, and then stand up with it while the objects should be as close to the body as possible;
- when carrying weights, try to distribute the load evenly, ie do not carry bags in one hand, etc. , if you have to carry an object yourself, keep it as close to your body as possible while not stretching your arms and use it to carry heavy loads, trolleys, bags or suitcases on wheels, backpacks;
- use a wide belt or special corset for heavy work involving lifting, moving or carrying weights;
- do not lift loads over 10 kg;
- when performing any work, try to bend and bend as little as possible and periodically relieve the spine (hang on the bar, stretch your arms raised, lying down);
- wear comfortable shoes; women should restrict walking in high heels.
- Exercise regularly to strengthen and maintain the corset. Swimming is useful.
- Take a contrast shower, temper the body.
- Do not overcool.
- Avoid scandals, stressful situations.
- Eat right.
- Do not smoke.



































