Osteochondrosis of the spine is a degenerative-dystrophic lesion of the intervertebral discs, the vertebral body, the ligament, in which the bone and cartilage tissue of the neck, chest, and lumbar spine are destroyed.
Pathology affects the entire motor segment of the spine, the disc, both vertebral bodies, and adjacent nerve and muscle structures. This disease is often referred to as the "disease of civilization" that is associated with vertical posture and stress on the spine every day.
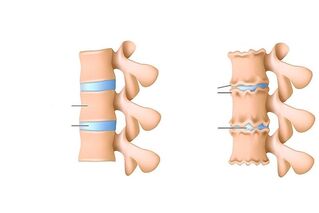
The main causes of spinal osteochondrosis are microtrauma during physical exertion, unhealthy diet, sedentary lifestyle, and even genetic predisposition. When this disease progresses, the intervertebral disc and adjacent structures suffer first. The central part of the disc changes, leading to a loss of the shock-absorbing properties of the vertebra, resulting in cracks and thinnings in the fibrous ring.
According to U. S. statisticians, the first reason for limiting the activity of people under the age of 45 is back and neck spine pain. The majority of urban residents, drivers who spend a significant portion of their time in a sitting position, refilling their spines, are at risk.
Osteochondrosis is the cause of more than 70% of back pain cases. The risk of the disease increases with age.
Etiology and pathogenesis of spinal osteochondrosis
Spinal osteochondrosis has a long-term pathogenesis (several months to decades). It depends on the factors that influence the development of the disease.
Risk Factors:
- Cor. Elderly people (over 60 years of age) are at risk. In people under 35, the disease is rare. Age-related changes result in disorders of the human hormonal background that make muscle tissue and vessel walls more porous, making them more vulnerable. This causes metabolic disorders, overloading the intervertebral discs.
- Autoimmune diseases that can perceive and destroy cartilage tissue as foreign.
- Spinal cord injuries. This is one of the main reasons for the development of osteochondrosis in young people. It is estimated that more than half of those with spinal cord injury at a young age suffer from osteochondrosis of the spine in old age.
- Overweight, which reduces wear on intervertebral discs. The discs serve as a kind of shock absorber for the spine, ensuring its mobility through physical activity, walking, running, and so on. During and protect bone tissue from destruction and the appearance of microcracks. The severity of the excess weight makes the load even stronger, which accelerates the process of disc destruction.
- Flat legs.
- Genetic predisposition.
- Diseases of the endocrine system that cause metabolic disorders, which in turn negatively affect the condition of cartilage tissue.
Osteochondrosis can be a "dormant state" for a long time. Many patients experience the disease in severe pain, when the dystrophic process in the cartilage tissue has already damaged the nerve roots.
There are stages in the pathogenesis of spinal osteochondrosis:
- Violation of blood circulation in intervertebral discs and adjacent structures.
- Hormonal and metabolic disorders especially in the body and intervertebral discs.
- Degradation processes of the nucleus pulposus. At this stage, the structure of the intervertebral disc changes - the nucleus shrinks, the disc itself becomes thinner, the load on the annulus fibrosus increases, leading to various stratifications, microcracks, and sometimes ruptures.
- Protrusion of intervertebral discs - protrusion of intervertebral disc tissue, often toward the spinal canal, on impact, causing severe pain.
- Intervertebral hernia. Progression of the protrusion leads to the destruction of the ligaments, changes in the height and shape of the disc, which in turn provokes the formation of hernias.
- Compression of radical arteries.
- Chronic insufficiency of blood supply to the spinal cord.
Symptoms of spinal osteochondrosis
With the development of osteochondrosis, pathologies appear in the intervertebral discs and in the cartilages themselves, which then overlap and can provoke the appearance of an intervertebral hernia.
Symptoms may be general and specific, characterized by abnormal changes in cartilage, intervertebral discs, and adjacent tissues.
The very first signs of osteochondrosis should be called aching back pain, numbness of the vertebral sections, limited movement, increased pain during physical exertion.
Specific symptoms of osteochondrosis:
- Cervical osteochondrosis is characterized by circulatory damage that causes dizziness, pain and tinnitus, and headaches. The brain is poorly enriched with oxygen and nutrients, resulting in a person experiencing a state of stress.
- The chest region is accompanied by osteochondrosis, often with intercostal neuralgia. There is pain in the chest and ribs.
- Osteochondrosis of the lumbar spine is caused by the development of diseases of the lumbago, lumbosacral (sciatica) and lumbar sciatica. In sciatica, the sciatic nerve is affected, pain and hypotension are observed in the buttocks, and hypotension in calves.
Symptoms of cervical osteochondrosis:
- Cirvicalgia - pain in the cervical spine. The nature of the pain is varied (dull, sharp, aggravated by tilting the head and torso when coughing), depending on what factor affects this section of the spine.
- Cervicobrachialgia - pain in the cervical spine, radiating to the hands, numbness.
- Shoulder-shoulder posterior and posterior inflammation - pain in the shoulder joint, clavicle, restricting arm movement from top to bottom.
- Epicondylosis - pain in the elbow joint, limited movement.
- Vertebral artery syndrome - called cervical migraine, head and neck pain, nausea, sometimes vomiting, impaired coordination of movements - shocking when walking, tinnitus.
One of the most common signs of osteochondrosis of the neck is impaired blood circulation, leading to frequent dizziness, fainting, and headaches.
Symptoms of osteochondrosis of the breast:
- Thoracalgia - chest pain, pain with immobility (occurs during prolonged sitting, at night), aggravated by physical activity, deep breathing, coughing.
- Heart syndrome.
- Posterior chest wall syndrome - pain in the area of the shoulder blades, pain sensations depend on the position of the body.
- First squalene muscle syndrome.
- Truncalgic syndrome - pain in half of the chest.
- Exacerbation of intercostal neuralgia.
Symptoms of lumbar osteochondrosis:
- Lumbodynia - pain in the lower back, lumbago. The patient feels discomfort when trying to sit or stand up. The pain is increased by physical activity, coughing, deep breathing, bending.
- Lumboischialgia - pain in the lower back that radiates to the foot. There may be paraesthesia, numbness of the legs, muscle cramps and joint pain.
- Vascular syndromes - debut by squeezing blood vessels, no pain, muscle weakness, cone syndrome - weakness of both feet, dysfunction of pelvic organs.
The symptoms of osteochondrosis of the lumbar spine are diverse. This part of the spine is more stressed than others.
Diagnosing spinal osteochondrosis
For the first back pain, an examination should be performed to determine the source of the pain. Osteochondrosis is a disease that is difficult to diagnose because pain can be caused by other pathologies not related to the spine. The patient will need the consultation of several specialists: a neurologist, primarily an orthopedist, a vertebrologist.
Methods for diagnosing osteochondrosis:
- Radiography. It is used to accurately determine the height of intervertebral plates or changes in the structure of vertebrae, changes in the diameter of holes between vertebrae. X-rays are most often taken in two positions - lying on your back and lying on your side. Two different projections of the images allow a more accurate determination of the presence of pathology. Sometimes an x-ray is taken of the lower jaw down.
- MRI and CT. MRI results are considered more accurate and help to quickly determine the localization of segments involved in the pathology, the presence or absence of intervertebral hernias, and root compression.
- Laboratory tests: a blood test to determine the level of calcium in the blood and the rate at which the erythrocyte settles. Laboratory tests are prescribed first, and more recently, based on these results, the doctor directs them to hardware diagnostics.
It is important to distinguish spinal osteochondrosis in a number of other diseases with a similar clinical picture, such as: oncological tumors of the spine, violation of cartilage tissue integrity, inflammation, intermittent claudication, cystitis in the internal organs, gastritis, urolithiasis, urolithiasis, , angina pectoris, nervous system disorders. For this purpose, studies of the digestive system, nervous system, and blood circulation can be prescribed. The following diagnostic methods are used - cardiogram, ultrasound, electroencephalography, endoscopic examination (digestive organs).
Complications of osteochondrosis
The course of the disease is most often accompanied by neurological complications:
- Section
- . Complications of protrusion - sharp painful shooting sensations.
- Stage. Radiculitis, characterized by pain syndromes and other symptoms, depending on the location of the radiculitis.
- Stage. Pathology of roots and spinal nerve, presence of intervertebral hernias. Muscle paresis often occurs, resulting in paralysis of the entire body.
- Stage. Violation of blood circulation and blood supply to the spinal cord. Symptoms: persistent severe back pain, paralysis of certain muscle groups, ischemic stroke of the spinal cord.
Treatment of osteochondrosis of the spine
The process of treating any type of osteochondrosis has a single goal - to relieve pain, prevent the destruction and deformation of spinal tissues. Treatment can be conservative or surgical. The type and mode of treatment is prescribed for each patient individually, based on the diagnosis (stage, type of disease, general well-being of the patient).
In the acute period of pain syndrome, relaxation and rest are recommended, anti-inflammatory drugs (dicloberl, voltaren), anticonvulsant mixtures, vitamin B injections, abrasives - dip rileaf, larkspur, etc. - may be prescribed as soon as the pain syndrome subsides. physical education and physiotherapy (diadynamic currents, electrophoresis, magnetotherapy).
Conservative treatment takes about two months. In addition to the listed treatment methods, massages, manual therapy, reflexology and extraction can also be used. The outcome of conservative treatment depends directly on the patient’s perseverance and diligence.
There is also a surgical treatment used in the presence of intervertebral hernas older than six months, compression of the roots of the spine due to narrowing of the gap between the vertebrae. The principle of surgical treatment is the removal of the deformed disc. The postoperative rehabilitation period is about six months. Rehabilitation includes exercise, physiotherapy and vitamin intake.
Preventing osteochondrosis of the spine consists of overcoming risk factors - maintaining an active lifestyle, exercising, proper nutrition, using a corset and special belt when loading the back, sleeping on orthopedic mattresses and pillows, avoiding hypothermia and injuries.



































