Pain in the hip jointThey are specific unpleasant, hard-to-tolerate feelings caused by the pathology of the upper femur, the acetabulum, nearby soft tissue structures. They become intolerable from the point of view of intensity, they can be boring, sharp, squeezing, aching, torn, drilled, etc. They often depend on load, time of day and other factors. The causes of pain are determined using X-rays, CT, MRI, ultrasound, arthroscopy and other tests. Painkillers and rest of the limbs are recommended until the diagnosis is made.
unpleasant, hard-to-tolerate feelings caused by the pathology of the upper femur, the acetabulum, nearby soft tissue structures. They become intolerable from the point of view of intensity, they can be boring, sharp, squeezing, aching, torn, drilled, etc. They often depend on load, time of day and other factors. The causes of pain are determined using X-rays, CT, MRI, ultrasound, arthroscopy and other tests. Painkillers and rest of the limbs are recommended until the diagnosis is made.
Causes of pain in the hip joint
Soft tissue injuries
The most common traumatic cause of pain is a contusion of the hip joint. Occurs when it falls to the side or has a direct effect, manifests itself in moderate acute pain that quickly becomes dull, gradually decreases, and disappears within a few days, in severe cases - weeks. The support is retained, movements are slightly restricted. Edema is detected locally, bruising is possible.
Injury to the ligaments of the hip joint is rare, usually as a result of road traffic accidents and sports injuries, accompanied by severe pain, sometimes a feeling of cracking (e. g. , from tissue tearing). The pain decreases somewhat and then often increases again due to edema. Swelling from the joint extends to the lumbar region, the thigh.
The dysfunction of the ligament of the ligament depends on the severity of the injury (stretching, tearing, cracking), ranging from a slight restriction to the inability to support the foot. The pain increases as the torso deviates, with movements in the opposite direction to the damaged ligament.
Bone and joint injuries
Hip fractures usually occur in older people as a result of domestic or street trauma. A characteristic feature, especially in the presence of osteoporosis, is the absence of intense pain syndrome, mild edema. At rest, the pain is deep, dull, moderate, or insignificant, with movements the painful feelings suddenly increase. Support is sometimes retained. A common symptom is the inability to lift a straightened leg from a predisposed position (a symptom of a stuck heel).
Transstrochanteric fractures are more commonly diagnosed in middle-aged and young people and develop as a result of high-energy trauma. Unlike neck fractures, they are accompanied by unbearable sharp, diffuse deep pain. After that, the pain decreases, but it is still very strong, difficult to wear. The joint is swollen and bruising is possible. Movement is severely restricted. Support is impossible.
Isolated fractures of the larger trochanter are rare; occur in children and adolescents; they are formed by a fall, a direct impact, or a sharp muscle contraction. The pain is acute, very intense, mainly localized on the outer surface of the joint. Due to the increased pain, the patient avoids active movements.
Displacement of the hip occurs during falls from a height, industrial and road traffic injuries, manifested in unbearable sharp pain that hardly subsides to the point of decline. The joint deforms, the leg shortens, bends at the knee joint, turns outwards, less often inwards (depending on the type of dislocation). Support and movement are impossible, if you try to move, determine the resistance of the spring.
Acetabular fractures develop in isolation or combine with hip dislocations. It is characterized by acute explosive pain deep in the hip joint. After that, the pain subsides slightly but remains intense, preventing any movement. The leg shortens and rotates outwards. Support is impossible.
Degenerative processes
In early-stage coxarthrosis, the pain is periodic, dull, of uncertain localization, appearing at the end of the day or after significant exertion, sometimes radiating to the hip, knee joint. Mild, rapidly transient stiffness is possible at the beginning of movements. After that, the intensity of the pain increases, painful feelings are perceived not only during movements but also at rest. After a great deal of effort, the patient begins to limp. Movement is somewhat limited.
In severe coxarthrosis, the pain is deep, diffuse, constant, sore, twisting. It disturbs both day and night. Decreases resistance to stress; when walking, patients lean on a comma. Movement is severely restricted, the affected leg shortens, leading to increased joint load, increased pain when walking and standing.
The process of chondromatosis of the hip joint resembles subacute arthritis. The pains are moderate, diffuse, transient, combined with crackling, limiting mobility. Injuries to intraarticular bodies result in occlusions characterized by intense sharp pain, impossibility of movement, or significant restriction. Once the joint mouse injury has been repaired, the listed symptoms disappear.
Trochanteritis usually develops with arthrosis of the hip joint, accompanied by an inflammatory-degenerative lesion of the tendons of the pharyngeal muscles at the site of their attachment to the larger trochanter, which manifests as pain in the area of the supine lesion. on the affected side. The pain intensifies when you try to kidnap your hips with resistance.

Eating disorders of bone
Perthes disease develops in children and adolescents and is characterized by partial necrosis of the femoral head, initially accompanied by intense, dull deep pain, sometimes radiating to the knees and hips. After a few months, the pain sharply intensifies, becoming permanent, sharp, exhausting. The joint swells, movement is restricted, and lameness occurs. Then the pain decreases, the degree of recovery of joint functions varies.
Aseptic necrosis of the femoral head is similar to Perthes disease when viewed downwards, but is detectable in adults, progresses less favorably, and is bilateral in half of the cases. At first, the pain is periodic, pull. Then the pain syndrome intensifies, appearing at night. At the height of clinical manifestations, the pain is so intense that the person completely loses the ability to lean on the foot. Then the pain gradually decreases. Restriction of movement progresses in about 2 years, resulting in hip arthrosis, contractures, and limb shortening.
Lone bone cysts develop in the proximal metaphysis of the thigh in 10-15 year old boys, accompanied by non-intense, intermittent pain in the hip joint. Edema is usually absent, and often prolonged course contractures develop, especially in young children. Due to mild symptoms, the cause of treatment is abnormal fracture or increasing restriction of movement.
Arthritis
Aseptic arthritis is manifested by wavy pain in the joint that intensifies in the hours before morning. The severity of pain, from insignificant to acute, severe, constant, significantly limits physical activity. Stiffness, swelling, redness and an increase in local temperature are observed. Feeling is painful.
In rheumatoid arthritis, the hip joints are rarely affected, the lesion is symmetrical. Intermittent pain first appears in the background of changing seasons (autumn, spring), with sharp changes in weather conditions, during periods of postpartum hormonal changes, or during menopause. The pain is moderate or weak, diffuse, pulling or sore, sharply increased on touch. It is combined with recurrent synovitis, edema, hyperemia, hyperthermia, increased restriction of mobility.
Infectious arthritis develops through the spread of a hematogenous or lymphogenic infection, and less frequently, through the penetration of the pathogen into a nearby tissue joint. Typically acute development with rapidly increasing painPain is intense, twitching, tearing, bursting, disturbing at rest, aggravated by movement, which puts the limb in a forced position. Patients are associated with fever, chills, sweating, severe weakness, edema, redness of the joint, and an increase in local temperature.
Without timely treatment, bacterial infectious arthritis can become panarthritis - a purulent inflammation of all tissues in the hip joint. It is characterized by a severe course with acutely widespread throbbing pains, hectic fever, severe weakness, pre-syncope condition, significant hyperemia, and hyperthermia.
Other inflammatory diseases
Upper thigh osteomyelitis can be hematogenic, post-traumatic, or postoperative. Hematogenous osteomyelitis is evident with localized, very acute rupture, twitching, tearing, or dull pain, as a result of which the patient avoids even the slightest movement of the limbs. There is significant hyperthermia, severe poisoning.
Post-traumatic and postoperative osteomyelitis occur with similar but less pronounced symptoms. Typically, a more gradual appearance in the background of an open fracture or postoperative wound, the appearance of purulent discharge. Hip pain increases within 1-2 weeks, in parallel with the progression of signs of local inflammation.
Synovitis develops in the background of injuries and other diseases of the hip joint, less often it is a manifestation of allergies. In acute synovitis, the pain is usually smaller, dull, ruptured, gradually increasing due to an increase in the amount of intraarticular fluid. The joint is swollen, slightly palpable to the touch, determining the symptom of fluctuation. Chronic synovitis is associated with asymptomatic, mild painful pain.
In the case of intermittent hydroarthrosis, the pain is also insignificant, accompanied by discomfort, limited mobility, and disappears within 3-5 days after the reverse absorption of the effusion. They recur at regular intervals, individually for each patient, caused by repeated accumulation of joint fluid.
Specific infections
Hip tuberculosis is a common form of osteoarticular tuberculosis, manifested by general weakness, fatigue, and subfebrile condition. Then there are weak pulling or aching pains in the muscles, there are temporary painful feelings in the joint while walking. The patient spares the limb. As the pain progresses, they are moderate, diffuse, radiating to the knee, accompanied by swelling, redness, and synovitis. A protective contracture develops.
Joint pain, including hip pain, can occur with brucellosis. In acute and subacute forms, painful feelings stretch and twist, combined with periodic fever, lymph nodes, skin rashes. In a chronic course, pain syndrome is similar to the development of deformities over time in aseptic arthritis.
Congenital disorders
Manifestations of hip dysplasia are determined by the degree of incongruence of the femoral head and acetabulum. With complete congenital dislocation, the pain appears immediately after the child begins to walk, accompanied by lameness. With moderate subluxation, painful sensations occur at the age of 5-6 years, which are directly related to the load on the foot.
With mild subluxation, the pathology is asymptomatic for a long time, and the pain syndrome manifests itself with the development of dysplastic coxarthrosis at the age of 25-30 years. Such arthrosis is characterized by a rapid increase in pain, early onset of pain at rest and at night, and progressive restriction of movement. All forms of dysplasia are accompanied by asymmetry of skin folds, the "click" symptom, and limited movement. In case of dislocation, shortening of the limb is observed.
Neoplasms
Typical asymptomatic course in benign tumors. The pain is minor, intermittent, and often does not develop over the years. Tumor growth is accompanied by a slow growth of pain syndrome, recurrent synovitis. Osteomas, osteoid osteomas, osteoblastomas, and chondromas are more commonly found in the hip area.
Malignancies (osteosarcomas, chondrosarcomas) are characterized by rapid progression of pain syndrome and other manifestations of pathology. At first, the pain is minor, short-lived, without specific localization, sometimes worsening at night. After that, they become sharp, durable, cut, surrounded, spread throughout the joint. The affected area is swollen and deformed. Weight loss, weakness, subfebrile condition. In advanced tumors, painful, unbearable pain is only eliminated with drugs.
Other reasons
Hip pain sometimes occurs in lumbosacral plexitis and sciatic neuropathy, but they are usually insignificant in the clinical picture of the disease, fading behind the background to intense pain in the buttocks and back of the thigh, limb weakness and tenderness abnormalities.
The pain syndrome of this localization is often observed in osteochondrosis and disc herniation. Pain can be detected in spondylitis, deforming spondyloarthrosis, and curvature of the spine. The pains are dull, intermittent, painful, often exacerbated during the period of exacerbation of the underlying disease. Their appearance may be due to permanent joint overload or the development of coxarthrosis.
Sometimes joint pain is caused by a mental illness or a depressive disorder. Diabetes is often accompanied by enthesopathies, capsulitis, and other lesions of the periarticular soft tissues. Possible drug arthropathy while taking certain medications.
Diagnostics
In case of injuries, diagnostic procedures are performed by traumatologists. Degenerative and inflammatory diseases are treated by orthopedists and rheumatologists. In the case of purulent processes, the involvement of surgeons is required. The investigation includes the collection of complaints, the study of the medical history, the physical examination, and further research. Taking into account the specifics of the pathological process, the following methods can be used:
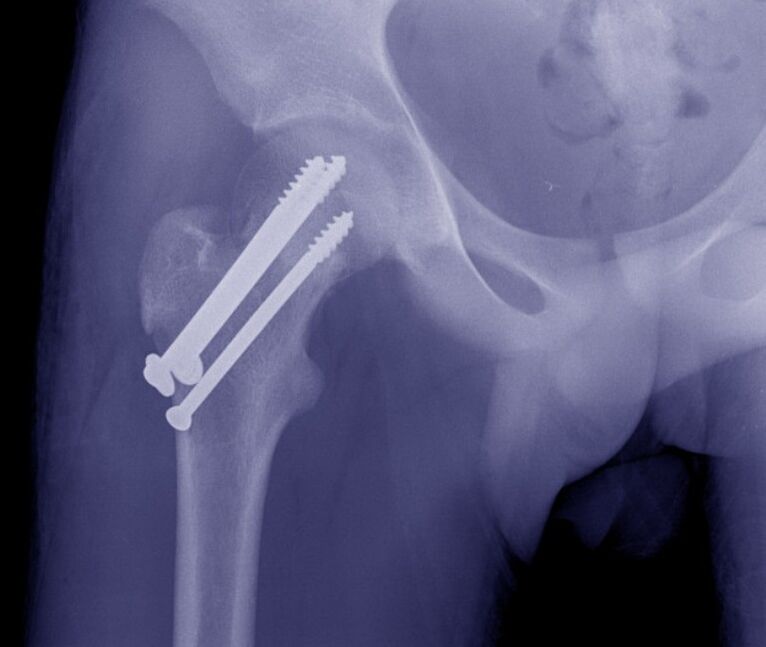
- Radiography.This is a basic technique for most joint diseases. It detects fractures, displacements, changes in the contour of the acetabulum and femoral head, marginal and intraosseous defects, bone growth, narrowing of the joint space.
- Ultrasound.It is most informative when studying soft tissues. It reveals the signs of inflammatory and degenerative processes, the areas of calcification. Effusion is used to diagnose joint mice.
- MRI and CT.Clarification techniques are used to clarify the nature, prevalence, and location of the abnormal focus in the case of ambiguous data from baseline studies. It can be done with a contrasting design.
- Defective joint.Diagnostic or therapeutic and diagnostic in nature. It allows the removal of the effusion, the study of the composition of the intraarticular fluid, and determines the pathogen of the infection with the help of laboratory tests.
- Arthroscopy.During the visual examination of the joint, the doctor assesses the condition of the bone and soft tissue structure, takes a biopsy sample for later histological examinations if necessary, and performs therapeutic measures.
- Laboratory tests.They are prescribed to determine the signs of inflammation and markers of rheumatological diseases, to assess the general condition of the body, the activity of various organs in the case of severe infectious or systemic pathologies.
Treatment
Help before diagnosis
In case of severe injuries, the joint should be secured using a splint from the foot to the armpit. For minor traumatic injuries, it is sufficient to rest the foot. Cold is applied to the affected area. In case of intense pain, an analgesic is given. It is not possible to perform active movements with the limb, to load the leg. It is strictly forbidden to prevent the displacement or displacement of the bones.
The tactics of non-traumatic diseases are determined by the symptoms. With minor manifestations, it is permissible to provide the rest of the limb, to use local analgesics and anti-inflammatory therapies. In case of fever, weakness, severe pain, rapid growth of edema and hyperaemia, it is recommended to seek immediate medical attention.
Conservative therapy
Dislocations indicate immediate reduction. In the case of fractures, skeletal adhesion is usually applied and then the patient is operated on, or the limb is fixed with drywall after signs of callus appear. In elderly patients with hip fractures, immobilization with derotation boots is permitted, which prevents rotational movements of the joint.
Other patients are advised to relieve the hip joint. It is recommended to use orthoses or additional devices (crutches, reeds) as indicated. Order massages, physiotherapy exercises, physiotherapy procedures
- laser therapy;
- magnetotherapy;
- UHF;
- ultrasound;
- electrophoresis with drugs;
- UHT.
Possible use of NSAIDs, chondroprotectors, antibacterial drugs. Topical agents are widely used. According to the indications, joint punctures, intra- and periarticular hormone occlusions, intra-articular injections of chondroprotectors, and synovial fluid substitutes are performed.
Surgery
Hip joint operations are performed using open access and arthroscopic equipment. Depending on the type of pathology, the following can be done:
- Traumatic injuries:open reduction of hip dislocation, acetabulum reconstruction, neck osteosynthesis, trochanteric fractures.
- Degenerative processes:arthrotomy, arthroscopy, removal of free intraarticular bodies.
- Tumors:removal of neoplasia, bone resection, disarticulation of hip joint, Io-abdominal amputation, Io-abdominal resection.
Contractures, ankylosis, periarticular tissue scarring, redression, arthroplasty and arthrodesis are performed. Endoprosthetics is an effective way to restore limb function in diseases of various origins, along with restriction of movement or destruction of the joint.



































